Monitoring the Health of Maui
The Maui Wildfire Exposure Study follows the health and recovery of Maui wildfire survivors.

Published: August 2024
It’s easy to overlook a cough, especially amid competing priorities like finding a job, tending to family, and searching for a home. But for Maui residents affected by August 2023’s wildfires, either directly or indirectly, that cough could be a symptom of deteriorating health.
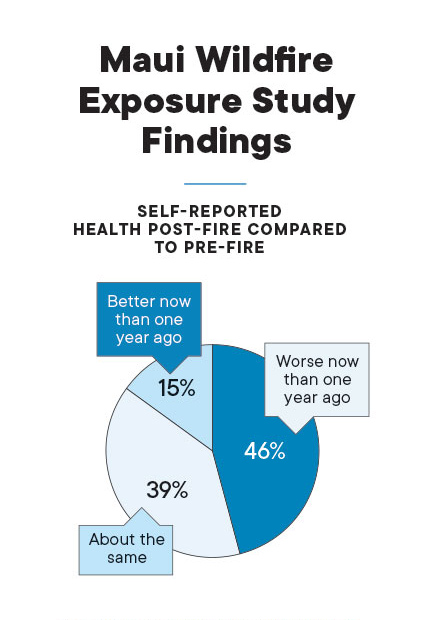
Forty-six percent of Maui residents surveyed reported that their health had declined in the past year, according to initial findings from the Maui Wildfire Exposure Study, or MauiWES. The survey was conducted by researchers at the University of Hawai‘i and funded by the Hawai‘i Community Foundation and Kaiser Permanente. It also reported that up to 60% of participants may suffer from poor respiratory health.
“It’s been really challenging for them to recover, because it’s not just one thing that will solve all of their problems. It’s a myriad of issues that they have to resolve to really not only recover, but to do so in a healthy way,” says Alika Maunakea, a professor at UH Mānoa’s John A. Burns School of Medicine, which headed up the study along with the University of Hawai‘i Economic Research Organization, or UHERO.
While the study, consisting of 679 participants, included the collection of biomedical samples, it also looked at social factors such as mental health, depression, suicidal ideation, and anxiety, as well as employment status, food insecurity, and access to care. The idea behind the study is to prevent long-term health issues among Maui’s survivors — and understanding the conditions in which they live, work, and play is a critical piece of that.
“This is the largest, most comprehensive study ever done in Hawaii after a disaster,” says Ruben Juarez, HMSA professor of health economics at UHERO. He is responsible for analyzing the study’s data and reporting its findings.
“If you don’t have good housing, if you don’t have a stable job, your priority is not going to be health,” says Juarez. “In fact, that’s what we’re seeing in our cohort, that many of these people… over 30% of people that we have in the study, this was their first medical check since the wildfire.”
The work of MauiWES is not just to collect data and analyze it, but also to monitor risk factors and inform participants of their medical results to help prevent any long-term problems.
“Without the support of Kaiser Permanente, we would not have been able to sustain this research project, nor expand to include a wider population,” Maunakea says. “Kaiser Permanente’s investment helped ensure that we will be able to continue this vital health research for the sake of our survivors and their future.”
Surprise findings
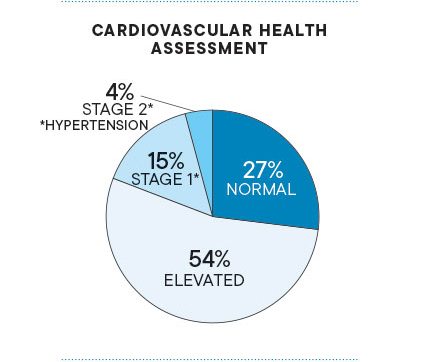
Maunakea knew the study would reveal respiratory health issues and increased cardiovascular risks. But, like Juarez, he didn’t expect that so many of the participants who were already showing symptoms weren’t seeing doctors. “They hadn’t gone to get a medical assessment or health assessment since the fires so that was surprising to hear,” Maunakea says. He explains that ignoring a cough due to exposure to ash and smoke could result in long-term lung problems and an increased risk for heart disease.
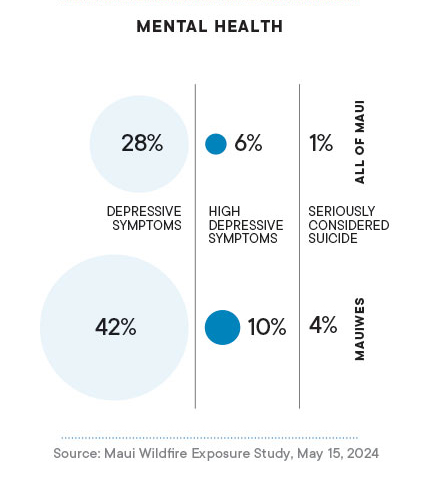
Maunakea was also surprised by the extent of the participants’ mental health issues. The study found that more than half of participants have symptoms of depression, with rates highest among middle-aged people. It also showed that 30% of participants have moderate to severe anxiety, 20% have low self-esteem, and 4.4% thought about suicide in the past month.
“Mental health impacts everything about your physical health and gets down to your physiology,” says Maunakea. “They all relate to each other. If you don’t get mental health support, your physical health might decline. If you don’t have access to care, then you’re less likely to take care of your health.”
Disparities in health insurance coverage were also found, with over 13% of participants lacking any health insurance at all. “That’s above the pre-wildfire average, which was about 5%,” says Juarez. “We’re seeing, for Hispanics, 38% don’t have health insurance and that’s something we’re actually working to address.”
Inclusion Matters
The wildfire exposure study is the first in Hawaii to include Hispanic representation on a social and biomedical scale. Hispanics make up 11% of Hawaii’s population, says Juarez, with the highest concentrations on Maui and Hawaii Island.
Community organizations engaged with minority groups to encourage participation in the study. “They’re just really grateful that they were taken into consideration,” says Veronica Jachowski, co-founder and executive director of Roots Reborn, a resource hub for Maui immigrants. The nonprofit helped MauiWES engage with over 200 people in Latino and Compact of Free Association, or COFA, communities.
In the study, more than 60% of Filipinos and Hispanic and Latinos reported very low food security. “Kaiser Permanente recognizes that food insecurity has worsened for survivors living in hotels and has stepped up to increase the amount of grants to community-based organizations supporting feeding programs,” says Jachowski. "This support makes a difference for families and individuals without access to kitchens or the ability to pay for groceries,” she says. The study also found that the Hispanic and Latino community has the largest number of residents without insurance, at 38%.
“If there’s representation in health studies, then you’re reducing biases,” Jachowski says. “If you have diverse representation, it helps researchers better understand how impacts, specifically fire impacts, affect different groups of people.”
Jachowski says that many of the study’s minority participants are extremely grateful for being included and for having their health results explained to them. “One of the things they always say is, like, ‘It’s good to know, otherwise how else would I have known? I don’t have insurance,’” says Jachowski.
“Kaiser Permanente’s Hawaii Health Access Program has provided critical access to individuals, the majority of whom are receiving access to health insurance for the first time in their lives,” Jachowski says. “This has completely revolutionized access for the most disenfranchised people of Maui.”
Expanding the study
With the initial report complete, Juarez and Maunakea say the goal now is to expand the cohort from 679 individuals to 2,000, including children for the first time.
Additional funding, which they are pursuing, could also provide an opportunity to extend the study an additional five years or longer. This would allow repeat screenings every year to look at some of the changes and update participants on additional findings.
Juarez and Maunakea are looking at the 9/11 World Trade Center Health Program’s ongoing screenings as a guide.
Participants want the support, says Maunakea. “They want to be included in the study over the long-term because they want to know what’s happening and make sure that they’re OK,” he says. “I think that really does help.”